Postcards from the EIS
By Martha McKenzie | Illustration by Michael Crampton

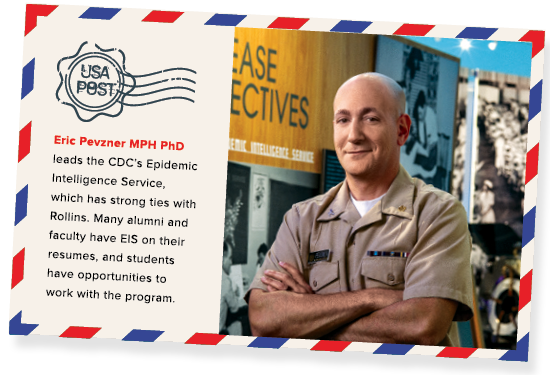
Rollins shares close ties with the CDC’s Epidemic Intelligence Service program. Students have opportunities to work alongside EIS officers, many alumni and faculty have served in the EIS, and Rollins epidemiology professors teach in the four-week course that kicks off each new class of EIS officers.
When Dr. Eric Pevzner was an MPH student in the late 1990s, one of his favorite courses was an epidemiology seminar that met every Tuesday morning down the street from Rollins at the Centers for Disease Control and Prevention. One week he might hear about a rash of unexplained hospitalizations in a rural town. The next he might listen to a discussion about the spread of a new disease in a remote region of Africa. And the next he could hear about response efforts to a catastrophic hurricane.
Pevzner was listening to the reports of the CDC’s Epidemic Intelligence Service (EIS) officers—the agency’s elite disease detectives. The officers in the two-year postgraduate fellowship are deployed to investigate disease outbreaks or natural disasters, knocking on doors, interviewing people, gathering and analyzing data to get to the bottom of the incidents. They work in anonymity—their names don’t make the headlines, but they are the first responders to the outbreaks that do.
Pevzner never lost his enthusiasm for the EIS program. Following his PhD, he went on to become an EIS officer in the Class of 2005. (The EIS identifies its classes by the year in which fellows enter, not graduate.) Then in June 2017, he assumed the helm as chief of the EIS program.
In many ways, Pevzner personifies the close ties between Rollins and the EIS program. Like Pevzner, many Rollins alumni go on to become EIS officers. Some of Rollins’ most well-known faculty have EIS posts on their CVs. MPH and PhD students have several options to work with the EIS program during their Rollins years. And new EIS officers spend their first four weeks in the program in Rollins classrooms taught in part by Rollins faculty.
“One of the things that makes Rollins unique is its extremely close connection with the CDC, and with the EIS program,” says Pevzner, who also serves as adjunct professor in the department of behavioral sciences and health education.
Each year, 500 to 600 professionals apply for between 60 to 80 positions in the EIS program. Rollins and Emory alumni claim a disproportionate number of slots. Between 2009 (the first year the EIS program began tracking the schools from which its officers came) and 2015, 70 of the 566 EIS officers who went through the program had an Emory degree under their belt. Of the 149 officers currently serving, 28 have at least one degree from Emory.
Perhaps all these Rollins alumni are drawn to the program because they’ve been taught by former EIS officers. To name but a few, Dr. Philip Brachman, Class of 1954, served as the second chief of the EIS from 1970 to 1981 and became a recognized anthrax expert during his time as an EIS officer. Brachman taught at Rollins until he passed away in 2016. Dr. Eugene Gangarosa, Class of 1964, founded the Rollins Center for Global Safe WASH. Dr. John McGowan Jr. was in the Class of 1969, and his daughter, Angie McGowan, was in the Class of 2002. Current faculty members with an EIS history include Drs. Ruth Berkelman, Patrick Sullivan, Scott McNabb, and Godfrey Oakley. Dean James Curran was named an honorary member of the Class of 2004 (and his daughter, Katie Curran, was in the Class of 2014). The list goes on.
Rollins students also have several opportunities to work directly with the EIS program. Through the Student Outreach and Response Team (SORT), students can help EIS officers with their disease response. During the Ebola outbreak, 45 SORT volunteers helped update the spotty maps of the affected areas with critical details such as exact locations of villages, roads, and buildings so responders could better direct their efforts.
More recently, the EIS reached out to SORT to help with contact tracing in a brucellosis outbreak in Texas traced to raw milk products from one dairy. Initially, brucellosis causes fever, aches, and fatigue, but if untreated, people can develop lifelong complications, such as arthritis and heart problems. “We needed to follow up with so many people in at least seven states who were potentially exposed to tainted products, but we just didn’t have the resources to do it,” says Pevzner. “The students were able to make a truly significant contribution to our effort. For the EIS program, SORT is an invaluable source of public health skilled labor.”
Students in the Rollins Earn and Learn (REAL) program can get posts with the EIS program. In this capacity, they might help with efforts to recruit EIS officers, plan and implement the annual EIS conference, and track outbreak investigations. “The Rollins REAL students contribute in many roles that allow this program to function as it does,” says Pevzner.
Rollins alumni who go on to become EIS officers will find themselves back in familiar territory. Each new class starts with a four-week course—sort of an epi boot camp—which is held on the Rollins campus. Three epidemiology professors—Drs. Patrick Sullivan, Michael Goodman, and Jodie Guest—teach some of the didactic portion of the course. “The fact that we have faculty who are doing cutting-edge epidemiological research to provide that level of teaching to our officers is a tremendous benefit to the program,” says Pevzner.
Rollins alumni have helped EIS disease detectives solve innumerable outbreaks. Here’s a look at a few:
Solving a foodborne outbreak
In 1988, the tiny rural town of Seneca, Kansas, was the site of the largest Campylobacter outbreak in the U.S. to that date. Most of the town, it seemed, was laid low with fever, nausea, and diarrhea.
To investigate, the CDC dispatched EIS officer Edwin Trevathan 82MPH/MD, who quickly figured out that everyone who had gotten sick went to the same church. “It was no great surprise,” he says. “I think almost the entire town was Catholic, and there was one big Catholic church.”

Edwin Trevathan MD MPH is professor of pediatrics and neurology at Vanderbilt University School of Medicine and director of the Vanderbilt Institute for Global Health. |
|---|
So Trevathan partnered with the church’s priests and attended all five services the following Sunday. At each service, the priest introduced Trevathan, explained why he was there, and instructed the parishioners to visit the tents that had been set up outside to answer a questionnaire and provide a stool culture. “The compliance rate was close to 100 percent because their priest told them to do it,” says Trevathan. “That was a big break for us.”
The questionnaires revealed that almost everyone who had become sick—or who had a positive culture but had not gotten sick—had attended a recent church picnic. Drilling down a bit more, almost all of them had eaten the homemade ice cream.
From there, Trevathan and colleagues were able to track which local dairy had supplied the unpasteurized raw milk for the ice cream and then isolate the individual cows that were infected. “I’m a city boy, and collecting a stool sample from a cow was not something I enjoyed,” he says. “But the overall experience was terrific. Many times, I’ve used the lesson I learned about involving the local church, synagogue, or mosque to reach people in the community. In fact, I’m using it right now for a project in Nigeria.
“What I have not used again is my cow stool culture technique,” says Trevathan. “That skill has gone to waste.”
Death in a dialysis clinic
Dr. Elise Beltrami 02MPH was finishing her first year as an EIS officer in 1996 when reports surfaced about an unusual cluster of liver failures and deaths at a hemodialysis clinic in northeastern Brazil. Problems had begun in mid-February, when several dialysis patients developed visual disturbances, nausea, and vomiting. Within a few weeks, a dozen patients had died of seizures or hemorrhages attributed to acute liver failure. By the time Beltrami arrived in early April, the death toll had climbed to 26, at least 20 others were hospitalized, and the outbreak had become front-page news in local papers.

Elise Beltrami MD MPH is associate director for Epidemiologic Science at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases and a commissioned officer of the US Public Health Service. |
|---|
Beltrami and her team began by tracking down and interviewing doctors, nurses, patients, and relatives of patients who had died—a task made harder by the fact that the clinic had closed by the time they arrived. They combed through medical records, dialysis records, autopsy reports, and laboratory results—all of which had to be translated from Portuguese. And they took water samples everywhere they went, including the local water treatment facility and the reservoir that served as the source of water for the community. People remembered that, around the time of the outbreak, there had been an algae bloom at the reservoir. “We suspected the problem was in the water,” says Beltrami. “And we were pretty sure we knew what it was— microcystin toxins. Lab tests showed we were right.”
Microcystin toxins are produced by cyanobacteria and are widespread in natural water sources. The toxins can kill animals that drink tainted water, but they generally just make humans sick. “The level of exposure was what made the difference,” says Beltrami. “Instead of drinking a cup of bad water, these patients had liters of it pumped into their bloodstream.”
In the end, 101 of 124 patients who underwent dialysis at the center during February 1996 had acute liver injury, and 50 died. That experience, along with others during her tenure with the EIS, convinced Beltrami to pursue a career in public health rather than internal medicine, as she had planned.
County fair flu
Dr. Yoran Grant-Greene 00OX 02C 06MPH was serving as a state EIS officer in Illinois in July 2012 when officials noticed an uptick in influenza-like illnesses and hospitalizations, particularly among children. It was early for flu season, but Grant-Greene recognized that the pattern matched those described by CDC reports in other states. The CDC in Atlanta confirmed the flu strain as H3N2v, a swine flu variant that was somewhat novel. This strain was highly virulent, incapacitating those it infected.

Yoran Grant-Greene MPH PhD is associate director for the West Africa region in the CDC’s Division of Global HIV and TB and a US Public Health Service officer. |
|---|
Armed with this knowledge, Grant-Greene and colleagues from the state health department sent questionnaires to hospitalized patients asking if they had had any contact with livestock or animals. It turned out nearly all the people who were sick with H3N2v, particularly the children, had been to a county agricultural fair within the previous week or two and been in direct contact with pigs.
“Some of the infected adults worked with pigs on their farms year-round, but not the children,” says Grant-Greene. “However, at the junior county fairs, the children were handling the pigs leading up to and especially on the day of the show. For children, the county fair was almost always the venue for infection.”
By mid-September, the CDC identified 306 cases of H3N2v influenza in 10 states. For Grant-Greene, whose work focused on HIV, responding to an emerging outbreak was fascinating, from both an epidemiologic and a public relations standpoint. “The outbreak could have been a huge drain on pig farmers’ businesses, so the whole state was saying, ‘No! You’re not going to shut down our industry!’” says Grant-Greene. “We had to be very sensitive and careful with the messaging.”
Legionnaires suspected and confirmed
Dr. Anthony (Tony) Fiore 98MPH was only a few days into the training program that kicks off an EIS officer’s tenure when he was called away to investigate what would turn out to be a textbook outbreak. It was July 1995, and residents of Chambersburg, a borough in rural south central Pennsylvania, were falling ill and dying of a respiratory illness.

Anthony Fiore MD MPH is chief of the Epidemiology Research and Innovations Branch, Division of Healthcare Quality Promotion, at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases. |
|---|
A few days after Fiore arrived, lab results confirmed the culprit was Legionnaires, the disease that was first diagnosed two decades earlier almost 160 miles away in Philadelphia. The diagnosis was a relief. According to Fiore, an Ebola outbreak was raging in Africa at the same time, so CDC staffers were edgy about an unknown respiratory virus that killed people. “We never really thought it could be Ebola here in the states, but just the same, it was reassuring when Legionnaires was confirmed,” says Fiore. Interviews with patients and families revealed that all of those who came down with the pneumonia-like symptoms were patients of or visitors to the local hospital or lived nearby.
All that remained was finding the source of infection. Was it outside the hospital at some nearby site, or was it in the hospital and being dispersed from there? Fiore interviewed people who were or had been ill, retracing their steps to find out when and where they had gone prior to getting sick. He tested the water at different sites, including the water in the huge cooling towers atop the hospital. “I remember climbing up the ladder to collect the water samples from the cooling tower thinking, ‘Well, this is different from anything I’ve done in my clinical training,’” says Fiore. “And I knew I would like to keep doing it.”
Fiore found the same strain of Legionella bacteria in the cooling tower water. The tower was cleaned and the outbreak contained, but not before Fiore was able to contribute to the understanding of the spread of the disease. Legionnaires is spread by airborne water droplets, but in the mid-1990s a faction in the medical community had begun disputing this. They believed instead that direct contact with contaminated water was necessary. One woman who got the disease lived a half mile from the hospital and had not visited it before she got sick. She did, however, sit and smoke on her front porch for hours each evening, reconfirming aerosol transmission.
Fiore’s three weeks in Chambersburg helped convince him to get his MPH in epidemiology from Rollins. He has investigated many outbreaks since, but he steers clear of the tall ladders.
In the aftermath of terror
As an EIS officer, Dr. Michael Martin 00MPH was assigned to the respiratory diseases branch, so he expected to spend his time investigating outbreaks of Legionnaires or pneumococcal pneumonia. But then terrorists flew two commercial airliners into the World Trade Center. “When something that big happens, everyone is called in,” says Martin.

Michael Martin MD MPH is senior technical adviser in the Division of Global HIV and TB at CDC Ukraine and a commissioned officer of the US Public Health Service. |
|---|
At the time, officials were concerned that the terrorists could launch a secondary chemical or biological weapons attack, so the CDC wanted to get boots on the ground as soon as possible. That’s how Martin found himself boarding a massive army cargo carrier with 29 other EIS officers and CDC volunteers in the early hours of the morning.
“All flights had been grounded at that point, and we were told that other than Air Force One, which was carrying President Bush to New York, we were the only plane in the air that day,” says Martin.
Upon arriving in New York, Martin and his colleagues split up to monitor the emergency departments in 15 hospitals throughout the city.
“We were looking for increases in key presentations, such as respiratory illnesses, severe illnesses—anything that might point to a bioterrorist attack,” says Martin, who was assigned to St. Vincent’s Hospital in Greenwich Village. “Thankfully, we did not find anything like that in the end.”
Coincidentally, Martin had been working at St. Vincent’s in 1993 when a bomb exploded in the World Trade Center‘s underground parking deck. St. Vincent’s was the referral hospital for the World Trade Center, so the staff cleared out the outpatient clinics to make a triage space for the casualties. Says Martin, “I remember thinking while looking down the street at those immense towers, ‘How could any terrorist think they could bring the Twin Towers down?’”
A mild virus turns deadly
Not all EIS investigations are able to be neatly resolved. Just ask Dr. Umesh Parashar 96MPH.
Parashar was in his first year in the EIS program in 1997 when there was a massive outbreak of hand-foot-and-mouth disease (HFMD) in Malaysia. This common childhood infection is characterized by fever, sores in the mouth, and rashes on the hands and feet, and it generally strikes children under the age of five. In most cases, the symptoms are mild, and children recover in a week or two without medical treatment.

Umesh Parashar MD MPH is chief of the Viral Gastroenteritis Branch in the CDC’s Division of Viral Diseases. |
|---|
However, in Malaysia, previously healthy children were becoming so ill with HFMD that they were being hospitalized, and at least 29 died of multi-organ failure within two days of being admitted. The outbreak was unusual enough to make international news, and the CDC reached out to Malaysian health authorities to offer assistance.
Parashar arrived shortly after the CDC’s offer was accepted. He spent nearly eight weeks working with the Malaysian authorities, visiting various hospitals that reported cases, and poring over hundreds of medical records from severe and fatal HFMD cases. He was looking for any clues that could explain why a traditionally benign virus turned deadly. Was there some other co-factor? Had some of the children been treated with different medications that might have exacerbated the illness? Did some have other medical conditions that made them vulnerable? Were severe cases clustered within a particular region with some common environmental exposure?
In the end, Parashar and local health officials were able to isolate the virus that caused the outbreak—enterovirus 71—but were not able to uncover why it ultimately hospitalized 889 children and killed 29.
“Likely, there was some unusual feature of this virus which had perhaps evolved over time that made it more virulent,” says Parashar. “But this is a case where we were just not able to pin it down.”
Riot epidemiology
On April 29, 1992, a jury acquitted four officers in the Los Angeles Police Department for the videotaped brutal beating and arrest of Rodney King. The verdict ignited simmering tensions between the LAPD and the African American community, setting off violent riots that lasted until the National Guard was able to quell them six days later.

Alexander Crosby MD MPH is senior medical adviser in the Division of Violence Prevention in the CDC’s Center for Injury Prevention and Control. |
|---|
In the aftermath of the disturbance, the LA County Health Department asked the CDC to send two teams. The first team focused on determining the scope of the intentional and unintentional injuries resulting from the riots. The second team worked with county officials to develop short- and long-term strategies to reduce violence. Dr. Alexander Crosby 91MPH was on the first team.
“Our job was to identify the injuries that were related to the civil disturbance versus those that had nothing to do with it,” says Crosby. “In a big city like LA, you are going to see a lot of knife, gunshot, and other injuries even if nothing else is going on.”
Crosby’s team called area hospitals to determine which received the most emergency room visits during the riots and identified four with the highest admissions. They then pored through their medical records to try to sort out the cause of the visits. Information was often hard to come by.
In the end, Crosby’s team estimated that about 25 percent of the injuries were related to the civil disturbance, including one in which the patient said that he had cut his arm on glass while looting. Another 25 percent were clearly not related to the riots, and the remaining cases could not be classified one way or the other.
“ERs are busy places,” says Crosby. “There isn’t a lot of time to write a lot of notes, so we were left to try to make as much sense of it as we could.”
Saving lives in Sierra Leone
Dr. Rebecca Levine 05MPH had just finished her EIS training in 2014 when she joined the first CDC team to travel to Sierra Leone to confront the Ebola epidemic. She arrived to a landscape of chaos and panic.
“There was so much fear,” says Levine. “Doctor’s offices and clinics were closing down and turning patients away. One of our burial teams, confronted in the street by fearful and frustrated families, had to abandon their truck full of bodies and come back later to retrieve it.”

Rebecca Levine MPH PhD is senior research scientist at the CDC. |
|---|
Levine was tasked with setting up a contact tracing system in Freetown, the nation’s capital. At the time, she was the only CDC person assisting the district health office for the city of more than 3 million people. She did not have access to a scanner or a copier, and cell phone coverage was spotty. There were only two Ebola treatment units in the entire country, and they were a seven- or eight-hour drive from the capital.
Despite the limitations, Levine trained local people already trusted in the community to be contact tracers. These tracers identified and contacted every person who had come in contact with an Ebola patient. She set up a reliable system to gather and update the data daily. “The only way we were going to get ahead of the outbreak was to be able to monitor all the contacts for 21 days,” says Levine. “I was able to set up a workable system in the month I was there.”
Levine was again deployed to Sierra Leone in December, but by that time Freetown had a small army of CDC and WHO epidemiology staff to assist the local surveillance officers. So Levine was sent to Kambia District, a remote, rural area near the Guinea border, where she re-created her contact tracing system. She returned to Kambia three more times, spending a total of 182 days in-country.
“Serving in Sierra Leone was one of the most life-changing things I’ve ever done,” says Levine. “To see what our colleagues there do with so much less than we have is humbling.”