On the front lines
By By Martha McKenzie | Illustration by Elliot Gordon

Rollins alumni in Georgia, the US, and across the globe are leading the way in responding to the COVID-19 pandemic. Here are just a few of their stories.
The race for a vaccine
Dr. Ami Shah Brown 00MPH is on the leading edge of the race to find a COVID-19 vaccine. Brown is senior vice president of regulatory affairs for Inovio Pharmaceuticals, which in early April began testing its vaccine in humans in a Phase 1 clinical trial.
“Inovio had a significant jump start,” says Brown. “We had the benefit of having an established platform and of having worked on a coronavirus vaccine for MERS.”
The platform to which Brown refers is the “infrastructure” of its vaccines. All of Inovio’s drugs begin with a DNA-based plasmid, a small, circular piece of DNA. “They all have the same backbone across every single disease we are trying to impact,” says Brown. “The only thing that is changed is a small piece of DNA that encodes whatever target you are looking for. All of our products have this same structure, and to date, they have shown very similar safety profiles in animals and in humans, so we have quite a database we were able to draw from to rapidly advance our COVID-19 vaccine candidate into clinical trials.”
|
|
Ami Shah Brown 00mph works for Inovio Pharmaceuticals, which is testing a covid-19 vaccine. |
Inovio also has a proprietary delivery device that enhances the uptake of the medicine. The device creates an electric field in the tissue being injected with the vaccine and follows up with short electrical pulses. Historically, DNA products without a delivery device have “worked wonderfully in the lab, but without direction to get into the cells, they just sit there,” says Brown. “Our device allows the DNA to get into the cells and elicit an immune response.”
The vaccine still has a long road ahead, Brown cautions, and that’s where she comes in. Her role is to help Inovio clear all the hurdles to bring the vaccine to the market. “I work with national and global regulatory agencies to understand licensure requirements to create regulatory pathways in various countries,” she says.
For example, in an appropriate circumstance, the US Food and Drug Administration has a mechanism to evaluate investigational products and approve them for emergency use. Given the COVID-19 pandemic, gathering the data that the FDA requires before Inovio’s vaccine could be considered for such use is important. “I have been thinking about these guidelines to make sure we can meet them in the event that this becomes possible,” says Brown.
Brown is currently navigating the vaccine’s development from her home, with her husband, Bruce Brown 01MPH, and their three school-age boys. “Working remotely has certainly added to the challenge,” says Brown, who sits on the Rollins Dean’s Council along with her husband. “But when this is finally over, I think you’ll see a lot more people going into public health.”
 The city streets were empty due to shelter-in-place directives.
The city streets were empty due to shelter-in-place directives.
Leading Atlanta’s response
When Atlanta Mayor Keisha Lance Bottoms appointed Dr. Angelica Geter Fugerson 10MPH as the city’s first chief health officer in July of last year, the goal was to address the heavy burden and disparities of the city’s HIV/AIDS epidemic.
Six months later, the first case of COVID-19 was reported in the US. The next month the virus became Geter Fugerson’s exclusive focus. She and Felipe den Brok, the city’s director of emergency preparedness, were tapped to lead the mayor’s Pandemic Coordination Team.
|
|
Angelica Geter Fugerson 10MPH advises atlanta Mayor Keisha Lance Bottoms on the city’s covid-19 response. |
“It’s an ever-evolving situation,” says Geter Fugerson. “It’s been about staying abreast of public health recommendations in research, identifying best practices in other cities, working with local clinics, and partnering with state and local health departments to make sure we are in alignment with their guidelines and messaging.”
Before joining the mayor’s office, Geter Fugerson served as a research fellow at the CDC, focusing much of her attention on HIV health disparities in the South. She has the same vulnerable population in her sights today. “The same people who didn’t have access to HIV resources are the same people who don’t have access to COVID-19 resources,” she says. “And while we know we have to keep people safe and flatten the curve, we also have to make sure people have food, that their utilities stay on, and that people who are homeless have access to resources.”
Toward that end, Geter Fugerson and her colleagues have worked with Mayor Bottoms to issue moratoriums on residential evictions and utility cut-offs. The mayor’s office created an emergency fund to support food programs for children and seniors, homeless preparedness, small businesses and hourly wage earners, and other areas impacted by COVID-19. The office has helped establish three testing sites in the city, with the goal of addressing ongoing racial and ethnic COVID-19 testing and treatment disparities.
While Geter Fugerson spends long days ensuring Atlanta residents and the mayor’s staff remain safe and healthy, she envisions a post-pandemic future. “The pandemic has reminded all of us to communicate with each other and partner like never before,” she says. “When this is over, I hope we see more integrated partnerships at the local and state level, more data sharing, more open communications. I’m excited to see what creativity comes out of this.”
Deploying the disease detectives
Dr. Eric Pevzner 98MPH PhD doesn’t remember the last time he had a day off. Pevzner leads the CDC’s Epidemic Intelligence Service (EIS)—the agency’s cadre of elite disease detectives. He and his team have been preparing for COVID-19 well before the first case made it to the US.
“We followed the reports of the virus’ spread in China and other countries in the region,” he says. “Given international travel, we knew it was just a matter of time before it came to the US.”
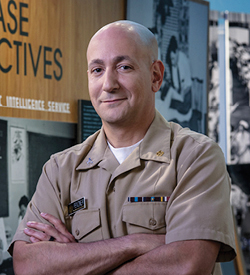
|
|
Eric Pevzner 98MPH leads the CDC’s Epidemic Intelligence Service. |
When the first cases did come ashore in January and February, EIS officers were on the scene investigating incidences, tracing contacts, collecting as much data as possible, and implementing control measures. Too quickly, they were forced to change gears. “Once we have community transmission of any pathogen, the jobs of EIS officers and all public health professionals become more complicated,” says Pevzner. “At some point, public health leaders must make the difficult decision to transition from containment to mitigation or slowing the spread.”
Normally EIS officers work all over the country on a wide variety of issues. During a pandemic, however, it’s all-hands-on-deck. All 130 EIS officers who can be deployed to help with COVID-19 response are, including Pevzner. He left Atlanta in mid-March to work on the front lines in Utah, where he remained until the end of April.
Responding to a pandemic such as COVID-19 is exactly what the EIS was created for. Since its inception in the 1950s, its epidemiologists have been among first responders in outbreaks around the world, including Ebola, SARS, HIV, and Zika. Before taking the helm of the EIS, Pevzner was deployed to combat the swine flu in Mexico in 2009 and Ebola in west Africa in 2015.
This pandemic, however, is different. “We have always been able to step into challenging situations, and then we could come back home and escape the situation,” says Pevzner. “There is no escaping this pandemic. It is a 24/7 response for the foreseeable future. All of our officers will be working on this every day until we can control the spread of the disease.”
On the scene of the first US case
Little did Marissa Cummings 19MPH know when she graduated from Rollins last spring that she would be thrown into the front lines of a pandemic eight months later.
Shortly after leaving Atlanta, she was hired as a high-consequence infectious disease (HCID) coordinator for Northwest Healthcare Response Network, a health care coalition that partners with state and local health departments and supports health care facilities in Washington State. In this role, she develops preparedness and response plans for any given HCID, traveling to facilities to conduct training and tabletop exercises. In fact, she had assisted in a training at Providence Regional Medical Center Everett three weeks before the facility admitted the first COVID-19 patient in the US.
|
|
Marissa Cummings 19MPH responded to the first cases of COVID-19 in the united states. |
Cummings immediately began working with the county and state health departments to help investigate. “They got access to CDC testing very quickly to confirm the case,” she says. “They did extremely detailed contact tracing to identify anyone who might have been exposed to that patient and had them self-isolate to avoid possibly infecting others. As far as we know, nobody that was exposed to that patient became infected.”
Nevertheless, Cummings and the public health community began working around the clock to prepare for the potential of more cases. A few weeks later, the virus surged through a long-term care facility, and then COVID-19 seemed to literally explode.
“After working with the facility that had the first patient, we were all preparing for what may come next,” she says. “But no one expected it to become a pandemic six weeks later.”
Cummings has since been spending her time working with health care facilities and colleagues at the University of Washington, collecting data on the number of COVID-19 cases in hospitals and ICUs, the facilities’ personal protective equipment supplies and needs, and their ventilator usage.
“Our governor is using the data we have collected to support his decisions in a phased reopening process and is constantly monitoring it to determine next steps forward or backward,” she says. “It’s been really amazing to witness the data collected from our partners being used in actual, evidence-based public health decision-making in Washington State.”